I have been hearing from several practitioners who are thinking of raising their rates. This is something that is necessary especially now given inflation. Before you decide to raise your rates, consider the following:
1) Why are you raising your rates? One thing to focus on more than raising rates is getting more patients AND patient visits. Are you doing a good job with scheduling supportive care visits long-term? How many new patients are you getting every week? Are you at your target weekly visits? If you are underperforming in those areas, then raising rates is NOT a good way to make up for it. And maybe it isn't time to raise your rates. Don't raise your rates if your clinic is underperforming. Fix that problem first.
2) Having more patients on the books can = lower increase in rates. If you have 400 patients a month and raise your rates by $5.00, that is not much of a shock to the patient, yet it means $2000 more revenue per month, and $24,000 more per year. When you have more patients, you can have a modest increase in rates and still make up a lot for inflation and increased costs.
3) Similar to #2, is your practice flow working? Are you working out of 1 room? Or are you running multiple rooms and multiple patients an hour? Having an ideal practice flow may mean the ability for a more modest rate increase while getting more bang for your buck.
4) Are your patients able to afford your services now? If patients are balking at coming in more than once per week, is it financial? If you are charging $150 a visit, is it realistic for someone to coming in 2-3 times per week for 3-4 weeks? And even if they start, are they going to finish? Or are they going to drop out of care and not finish their treatment plans? Again, have an efficient practice and you can see more patients, charge a rate they can handle, see them more often and get the revenue you need. It's a win-win. (keep in mind a lot of patients claim they are broke and they aren't, but there is a tipping point and most people are paying out of pocket).
5) Cutting expenses first: Anthony mentioned this in his post above. We get lost with our subscriptions and not shopping around for better rates on things like insurance. It is easy to save $30, $50, or $100 or more per month. Just DON'T cut your subscription to the locals community since it actually makes you money. 🙂

January’s webinar is here! This one is a favorite of mine because it includes the fascial lens when teaching the movement of the foot and ankle. It cover anatomy, fascia, and accessory motion of the foot and ankle. Definitely worth checking out.
Give this a read after you watch the video: https://pmc.ncbi.nlm.nih.gov/articles/PMC7689775/
Join us Saturday February 28th at 12:30 pm EST!
Live lab is back this Saturday! Let’s nerd out together! 🤓
NOTE: registration is required 👉🏽 https://us02web.zoom.us/meeting/register/T0US6enHT5ywbo-ebRN_IQ

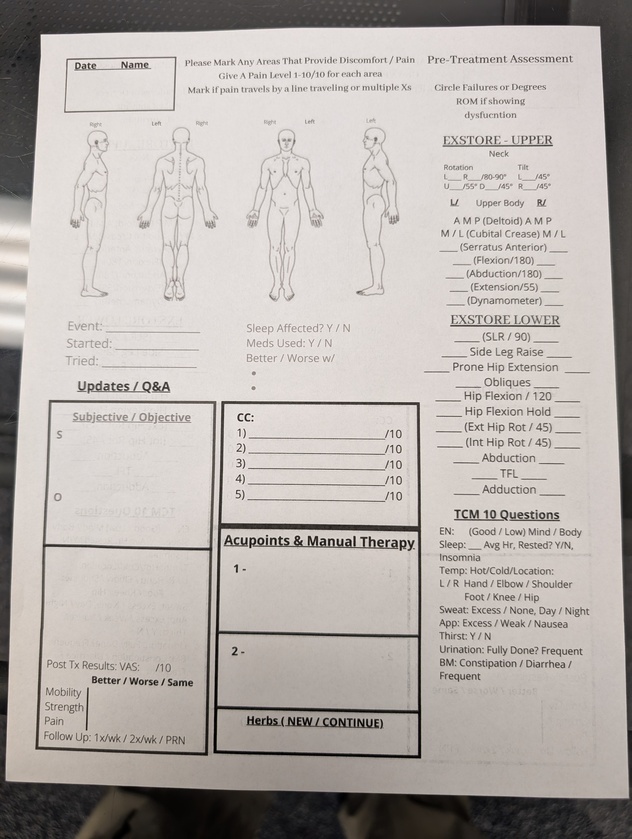
@Exstoreman 62 year old female with Left Lateral Leg Pain. Constant pain radiating down lateral left thigh and calf into foot with numbness and cold feeling primarily in big toe and pins-and-needles sensation throughout upper foot. Whole foot is very sensitive. Leg feels heavy.
Began 2 years ago with sudden severe low back pain. Toes in L foot suddenly went numb and went up side of leg.
See attached MRI report.
She's otherwise very healthy and has NO LBP whatsoever. Walks 4-5 miles/day. Skis (and notices it’s harder to turn with left leg).
Have treated her 5 times so far (weekly), treating MPs and doing renovation with no improvement in symptoms except for after the 3rd visit her leg felt a bit lighter, but just for a few hours. Also, SLR is improved.
Wondering if there's anything else I can try? MRI mentioned drop foot (no symptoms now) - should I treat the peroneal nerve (as discussed in recent LIVE)? Other ideas?
1st EXSTORE Scan:
ROM:
SLR: L-50 / R-60 (limited by hamstring tightness)
Inhibition:
- L TFL
- R ...