A 15 year old girl developed R shoulder pain one year ago after sleeping on it weird. Pain is constant and unable to raise hand above shoulder height (for instance raising her hand in school to ask a question).
3 months after the onset she had a diagnostic ultrasound which found a small supraspinatus tear (rotator cuff muscle). She then had 24 physical therapy visits over 12 weeks with no improvement. 2 months later she had a shoulder MRI - this did NOT show a supraspinatus tear.
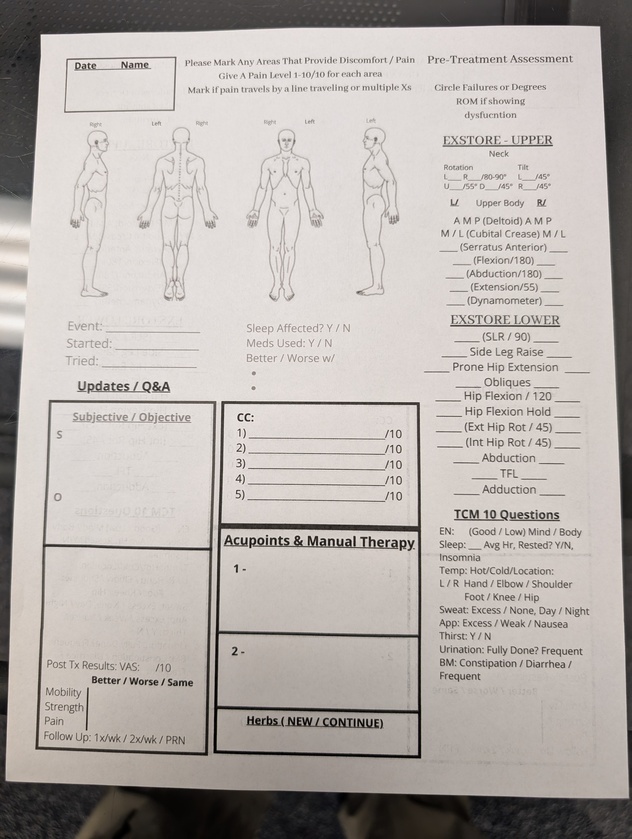
11 months after initial onset the patient was referred to me. Pain was still constant (10/10 on VAS) EXSTORE exam was as follows:
•unable to flex shoulder above 90 deg on R
•scapular stability (serratus anterior) on R is inhibited
•during testing of serratus anterior upper trapezius is in spasm
•c spine ROM to the left is 45 deg
•patient cannot do any pushup or modified pushup in school gym class.
•Patient is afraid of needles.
TREATMENT
•the patient agrees to only one needle with some convincing from her mother but does NOT agree to Pointer Plus stimulation.
•I insert needle into serratus anterior with a twitch response - and leave for 30 seconds then follow up with some manual fascial release to the mid axillary line.
RESULT
The patient was off for Christmas for 2 weeks and when she returned she reported her shoulder was 80% less painful (2/10 of VAS)
•shoulder flexion improved to 170 degrees and the scapular stability was 100% stable on EXSTORE re-exam. Her c spine ROM was now 80 deg rotation bilateral.
DISCUSSION
Being specific with your assessment will pay dividends. Take diagnostic imaging into consideration but do not lean on it - do a functional exam. For a joint to move you need two things: muscles to stabilize the joint being moved and muscles to do the moving. This is why learning to assess and treat the serratus anterior is non-negotiable when aspiring to become consistently proficient in treating shoulder and neck dysfunction. This girl had 24 visits with another therapy. 24 visits! Clearly those therapists didnt know what they didnt know. We have the tools and its easier than you think folks.
January’s webinar is here! This one is a favorite of mine because it includes the fascial lens when teaching the movement of the foot and ankle. It cover anatomy, fascia, and accessory motion of the foot and ankle. Definitely worth checking out.
Give this a read after you watch the video: https://pmc.ncbi.nlm.nih.gov/articles/PMC7689775/
Join us Saturday February 28th at 12:30 pm EST!
Live lab is back this Saturday! Let’s nerd out together! 🤓
NOTE: registration is required 👉🏽 https://us02web.zoom.us/meeting/register/T0US6enHT5ywbo-ebRN_IQ

@Exstoreman 62 year old female with Left Lateral Leg Pain. Constant pain radiating down lateral left thigh and calf into foot with numbness and cold feeling primarily in big toe and pins-and-needles sensation throughout upper foot. Whole foot is very sensitive. Leg feels heavy.
Began 2 years ago with sudden severe low back pain. Toes in L foot suddenly went numb and went up side of leg.
See attached MRI report.
She's otherwise very healthy and has NO LBP whatsoever. Walks 4-5 miles/day. Skis (and notices it’s harder to turn with left leg).
Have treated her 5 times so far (weekly), treating MPs and doing renovation with no improvement in symptoms except for after the 3rd visit her leg felt a bit lighter, but just for a few hours. Also, SLR is improved.
Wondering if there's anything else I can try? MRI mentioned drop foot (no symptoms now) - should I treat the peroneal nerve (as discussed in recent LIVE)? Other ideas?
1st EXSTORE Scan:
ROM:
SLR: L-50 / R-60 (limited by hamstring tightness)
Inhibition:
- L TFL
- R ...